Commercial Building Pressurization – Air Pressure
Why Building Pressurization Matters
In commercial construction, one often overlooked aspect of planning and design is keeping a building in a homeostatic state in terms to air pressurization. The reason for this is simply that, there are a lot of variables that can affect a building’s air pressure that can not be accounted for.
There exists many unaccounted for variables that affect a buildings air pressure which can cause it to function much differently than the way it was originally designed or engineered. Abnormal foot traffic patterns, causing doors to be opened more than anticipated is one of the more obvious ways. Natural degradation of building materials and/or poorly functioning HVAC systems is another; albeit this may take years to be noticible. Even something as simple as not changing air filters in the HVAC blowers can affect the pressurization of a building. In any case, the inability to create or maintain a homeostatic building pressurization can cause a multitude of issues.
Poor Building Air Pressurization = Poor Air Quality
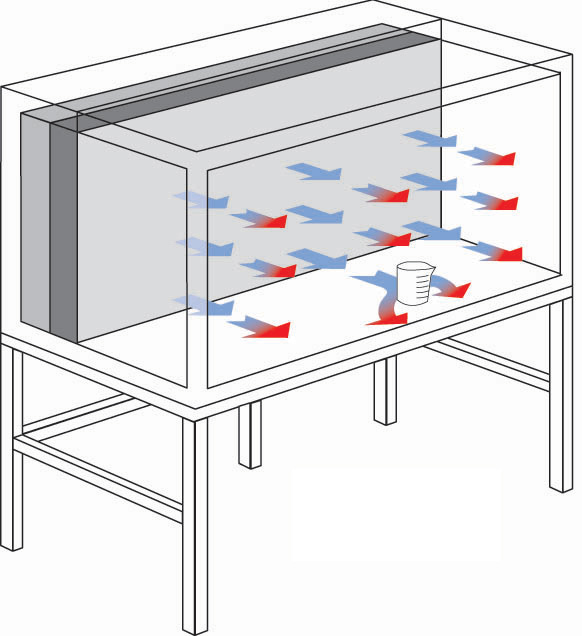
Most buildings attempt to maintain an environment of positive air pressure. In short, this means there is greater or “higher” pressure inside the building than that of the outside atmospheric resting pressure. This serves a few basic functions. It ensures that dust, dirt and debris introduced into a building is “pushed” back out once a door or window is opened. You probably experience this when you enter a commercial building. In most commercial buildings, when the automatic door opens you typically feel a rush of air exiting the building. That air can be likened to deflating a balloon – the pressure in the balloon seeks to deflate to an area of lower pressure – so the balloon air rushes out.
This air moving into or out-of a building is due to the pressure differential. If the air pressure in the building is greater than the air pressure outdoors, it is called a “positive pressure room” or “positive air pressure building.” Conversely, if the pressure inside the building is less than the pressure outdoors, the room or building is said to have “negative pressure.” Generally it is not desirable to have negative pressure inside a building. The problem with negative pressure is that once a door or window is opened – any exterior air is permitted to enter the building. That unfiltered air brings with it pollen, dust, dirt, biological and chemical particulates, etc. These particles entering the building and affect the people working in the building and the general cleanliness of the building.
Filtration For Cleaner Air
Keeping the air fresh in a positive pressure building requires precise engineering. To keep a building pressurized requires air to be drawn into the building to create the positive pressure. Since it is not being pulled from undesirable sources like unfiltered air via doors and windows – it must be pulled from an outside source across a filtration system.
HVAC systems pull air from a fresh air duct and through various types of filters. The more fine the filter media the more force required to pull the air across it. So the more robust the HVAC system will need to be. This is like sucking a milkshake through a straw with a tiny diameter. Now, let’s imagine a person sucking the same milkshake through a very large straw. Same concept – more suction/blowing power is needed to pull more air through more filters or finer filters.
And how tight or leaky a building is will determine the amount of air per cubic foot per minute to inflate the building envelop (balloon). Some buildings require as little as 45 CFM per 1000 SqFt. Other, more drafty or leaky buildings may require up to 300 CFM. The amount of air needed to positively pressurize and maintain pressurization will initially affect the design of the building HVAC system, and after the building is completed, the energy costs. It is much better to seal up air leaks in a building than to use larger fans to ‘push’ more air into a leaky building to maintain a positive pressure.
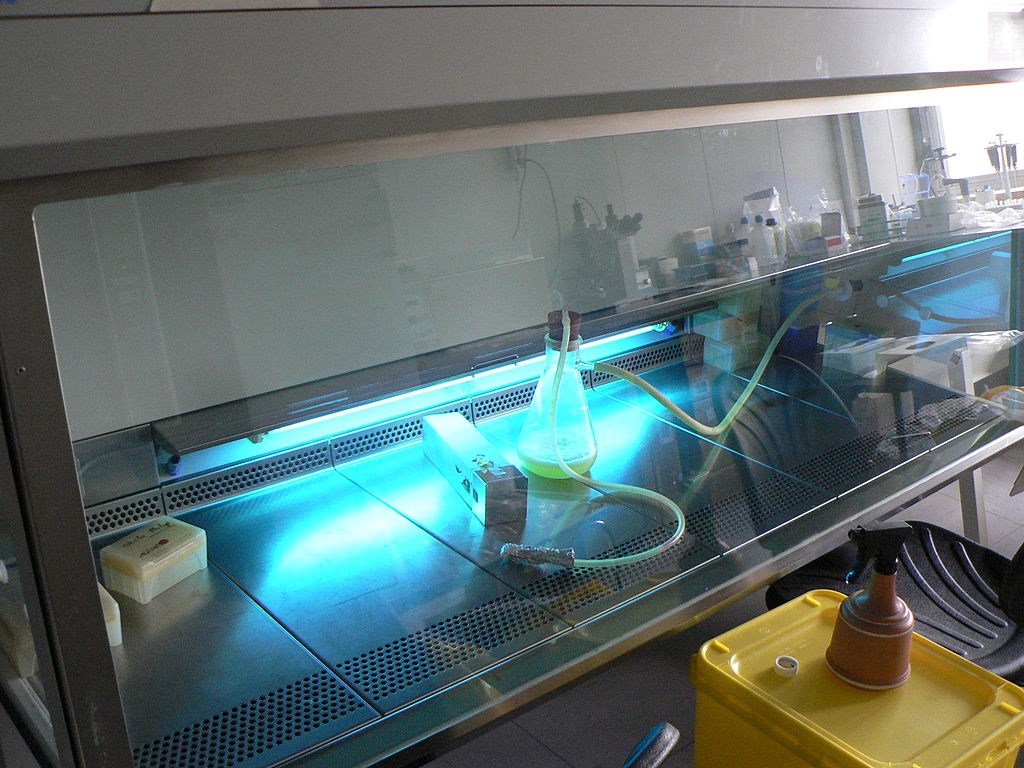
Negative Pressure Areas
Even in the most strict of positive pressure room and building environments you will want areas of negative pressure. These include maintenance closets, bathrooms, food prep areas, areas where chemicals are used, etc. In these areas, it is important to create negative room or area pressure so the fumes exit these areas quickly. To create they localized areas of negative pressure exhaust fans can be used very effectively. Once installed they will function to relive the area of polluted air, and at the same time, allow an equal volume of clean air to constantly flow into the area.
It is important from an engineering perspective to refill the area of negative pressure with an equal volume of clean air. This air is called “make up air” – or “air that makes up for the deficit of air created by the exhaust.” The overall building HVAC system must be engineered and calibrated to account for these deliberate breeches in positive air pressurization.
Monitoring results
Because there are areas of positive and negative pressure inside a building it is not possible to measure “building pressure” at any one spot. Different rooms and areas have different pressures – some positive and some negative. It is much more important to think of local pressure. In a hospital, for example, it might be important to have negative pressure in patient’s rooms but positive pressure in lobby areas. It is critical, in fact even mandated by federal laws and local codes, to have negative pressure in areas of nuclear medicine. The system of maintaining positive and negative air pressure is a very complex process, more art than science in many cases. However, it is an important concept to understand. Just because a building “feels” like it has positive air pressure in no way means it is acting the way it should. This is where it is critical to ensure absolute certainty that a each area of a building’s air pressurization system is functioning properly. in fact, if it is not working properly – it can cost hundreds or even hundreds of thousands of dollars in operating costs, depending on the size of the building.
Simple yet effective systems exist that can either be integrated with existing building management and control systems and/or act as standalone monitoring systems for room air pressure. Some of these systems are capable of monitoring both negative and positive air pressure and in multiple rooms simultaneously. Even further, some systems allow for monitoring of temperature and humidity – both of which are complimentary variables in overall environmentally controlled rooms and especially in positive and negative air pressure rooms.
Installing many of these systems requires little or no technical experience and can be set up and running out of the box in a few minutes. The advantage of using some of the more reliable systems on the market is the ability to alerting one or more building maintenance personnel of issues before they are in a “no turning back” scenario. In such systems, authorized building personnel can receive alerts via test/SMS messaging, email alerts, and even phone calls. In essence, if there is too little pressure in a controlled environment, it means the company is spending more money in wasted energy to maintain positive pressure. If a system were put into place to monitor positive pressure, there would be no more doubt and even better – no more wasted money.
Keep this in mind next time you receive your heating and cooling bill. It may well be that lowering energy cost is a simple fix – but one you’ll be able to realize unless you are certain what your current environmental conditions are.